| Health / Health News |
Combination targeted treatment produces lasting remissions in people with resistant aggressive B-cell lymphoma
Researchers at the National Institutes of Health (NIH) have developed a non-chemotherapy treatment regimen that is achieving full remissions for some people with aggressive B-cell lymphoma that has come back or is no longer responding to standard treatments.
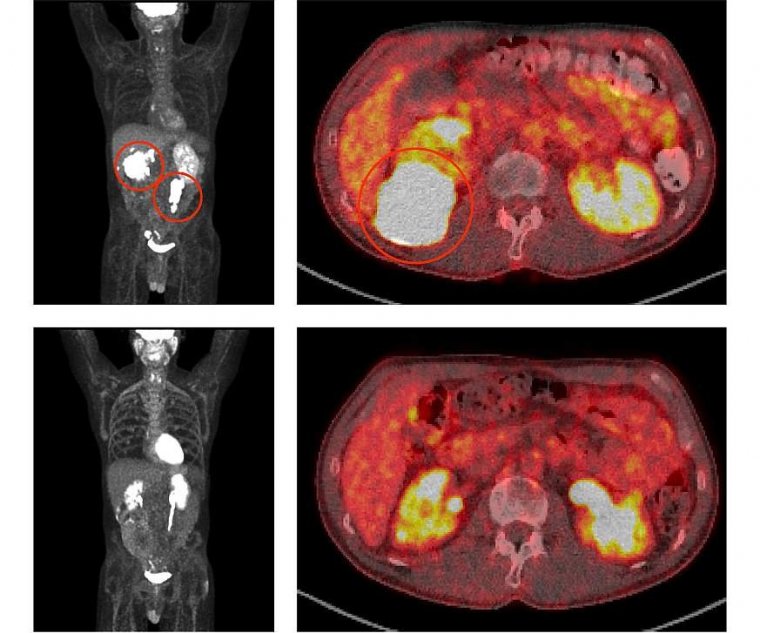
Before treatment with ViPOR, full-body and cross-sectional PET scans of a patient show large lymphoma tumors (circled in the top two panels). Following treatment, the tumors have disappeared (bottom two panels). Photo: Center for Cancer Research/National Cancer Institute
The five-drug combination targets multiple molecular pathways that diffuse large B-cell lymphoma (DLBCL) tumors use to survive.
Researchers at the National Institutes of Health (NIH) have developed a non-chemotherapy treatment regimen that is achieving full remissions for some people with aggressive B-cell lymphoma that has come back or is no longer responding to standard treatments.
The five-drug combination targets multiple molecular pathways that diffuse large B-cell lymphoma (DLBCL) tumors use to survive.
In a clinical trial at NIH’s National Cancer Institute, researchers tested the combination of venetoclax, ibrutinib, prednisone, obinutuzumab, and lenalidomide (called ViPOR) in 50 patients with DLBCL, the most common type of lymphoma.
The treatment shrank tumors substantially in 26 of 48 (54%) evaluable patients, with 18 (38%) of those patients’ tumors disappearing entirely, known as a complete response.
At two years, 36% of all patients were alive and 34% were free of disease. These benefits were seen mainly in people with two specific subtypes of DLBCL.
“Many of these patients who stopped responding to standard treatments would have otherwise died within a year, and now we have a good proportion who are still alive past two years, and some past four years,” said Christopher J. Melani, M.D., of NCI’s Center for Cancer Research, who co-led the study.
“It’s gratifying to see these long-term remissions and potential cures in patients.”
Previous studies have identified various genetic pathways involved in the development and survival of the different molecular subtypes of DLBCL, such as activated B cell–like (ABC) DLBCL and germinal center B cell–like (GCB) DLBCL.
Targeted drugs have shown effectiveness in blocking some of these pathways, but individual drugs rarely produced lasting responses in patients because the tumors may be resistant due to alternative survival pathways.
Dr. Melani and his colleagues hypothesized that combining targeted drugs that block multiple survival pathways would lead to more durable responses.
Based on laboratory studies in which they analyzed which targeted drugs could best be combined to kill DLBCL cells in a synergistic manner, the researchers designed the five-drug regimen to test in human trials.
To allow for the targeted drugs to work synergistically in patients, the researchers gave the drugs simultaneously in two-week cycles. To limit the accumulation of side effects, they scheduled a weeklong break between each cycle.
DLBCL is one of the most genetically heterogeneous forms of cancer, and as a result we don't yet have the ability to identify exactly which combination of drugs would be most effective for any given patient,” Dr. Melani said. “By putting five drugs together, we believe that there will be some drug combination—either two, three, or more drugs—that will be particularly effective against that patient's tumor.”
In the phase 1b/2 trial, 50 people with DLBCL that had relapsed or stopped responding to treatment were given six cycles of the ViPOR regimen. Responses to ViPOR varied by DLBCL subtype, with complete responses concentrated in two subtypes, including in 8 of 13 (62%) people with non-GCB DLBCL and 8 of 15 (53%) people with a form of GCB DLBCL known as high-grade B-cell lymphoma “double hit.”
At two years, people with non-GCB DLBCL and double-hit GCB DLBCL had higher rates of both progression-free and overall survival than other people in the study.
Non-GCB DLBCL and double-hit GCB DLBCL are highly reliant on the survival mechanisms targeted by ViPOR, so it makes sense that they responded particularly well to the combination therapy.
ViPOR also helped 6 of 20 (30%) patients whose lymphomas had not responded to or had come back after CAR T-cell therapy—the current standard of care for people with relapsed DLBCL—achieve lasting remissions.
Side effects of the five-drug regimen were generally mild to moderate when compared with those of standard treatments and improved during the treatment breaks.
Only five patients had to stop treatment early for various reasons, including side effects. Given these relatively mild to moderate side effects, additional drugs could potentially be added to ViPOR to improve its efficacy, the researchers said.
The team is also studying the ViPOR regimen in people with other types of lymphoma that are resistant to previous therapies.
The researchers have developed a larger phase 2 study, which will be conducted at multiple centers, to confirm the activity of ViPOR in people with non-GCB DLBCL and double-hit GCB DLBCL.
More work is needed to develop therapies for GCB DLBCL subtypes that aren’t as responsive to ViPOR.
YOU MAY ALSO LIKE





